News
Rare is not so rare
I want to find a treatment for a disease. The disease is inevitably fatal within the first months of life, but it is rare. It only affects one in one million live births. So, why should we care? Well, the disease I am looking at is only one of about 7,000 rare diseases. In total, about 3.5 million people in the UK are affected by a rare disease. In the end even for the rarest diseases children are being born every day who will say “I am the one, the one in a million”.
In the disease surfactant protein B deficiency, a certain protein called surfactant protein B is missing in the lung of new-born babies. The lung is lined with a thin protective layer of proteins and lipids. If surfactant protein B is absent, this layer destabilises the lung at the end of exhalation and the lung collapses. Surfactant protein B is absent from these babies’ lungs because the body’s genetic information, also known as DNA, is damaged. DNA is like a book of instructions that tells each cell in your body how to make all the components necessary for life. In babies with this disease, the instructions to make surfactant protein B have flaws known as mutations, so the cells of the lung cannot make the protein. Surfactant protein B deficiency is a recessive genetic disease meaning that patients are healthy as long as one of the two gene copies in a person is functional. The most common mutation is the insertion of two additional DNA units in the genetic code which accounts for about 66% of all cases. The mutation causes a premature ‘stop’ in the code and the instructions for protein synthesis are too unstable for the protein to be produced at all. New-born babies with surfactant protein B deficiency cannot breathe after being born and children die within their first months of life. The only available treatment is transplanting a lung from another child which is a rarely attempted, very high-risk procedure. Hence, for babies born with this disease, the odds of surviving, even for a year, are very low. We know exactly what the problem is, but still cannot treat the disease – isn’t that frustrating?
Fixing the fluid layer, and hence the babies’ lungs, would solve the problem. If we know that the fluid is not working because a component is missing, couldn’t we fix it by adding it back in? That is my project.
I am trying to use a technique called ‘gene therapy’ to overcome this. The idea is that we deliver the correct instructions back to the lung cells, so that they can make the correct fluid component. This is the only way to fix the lung because administering the missing protein itself to the lung is ineffective. The concept of gene therapy for this disease is shown in Figure 1.
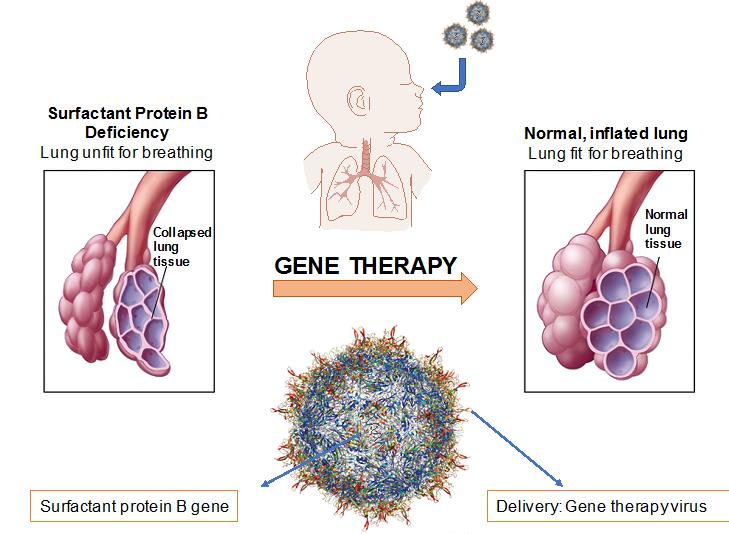
Figure 1. Schematic of gene therapy for surfactant protein B deficiency. A gene therapy virus is used as a vehicle to deliver the missing surfactant protein B genetic information to the patient’s lung. Gene delivery allows for a normally inflated lung and breathing in the patients.
Gene therapy is not easy. The first question is: how do we design genetic instructions on how to make the protein in the clearest possible way so that cells understand what component they have to make? This is one big part of my project.
The second big question is: how do we deliver the instructions to where they need to be, in the cells of the lung? To do that, we need to choose a suitable transport vehicle. In my project, I am looking at using viruses. A virus’ everyday job is to sneak under the radar of the immune system and deliver their own genetic material to cells in the body to infect them. Why not take advantage of this system?
I am investigating a modified version of a virus called adeno-associated virus. These gene therapy viruses were altered so that they cannot cause harm and they have been safely used in patients before. Adeno-associated viruses can have different types of surfaces, which determines what cells they are able to enter. In my project I want to select the gene therapy virus with the surface that is the best at entering the cells in the lung that have the ability to produce surfactant protein B. These cells are called alveolar type II cells and are found in the region of gas exchange in the lung.
Once I Identified the best set of genetic instructions and the best virus surface for delivery, I can assemble my gene therapy virus. To find out if it can actually treat the disease, I will first test my gene therapy virus in mice which have damaged surfactant protein B DNA, exactly as in the little patients.
With my project, I want to lay the foundation for a long journey to develop a new drug. The goal is to provide treatment for patients with surfactant protein B deficiency and therefore being able to treat one more of the 7000 rare diseases. However, surfactant protein B deficiency is only one of four disorders where components of the lung lining fluid are missing, so hopefully my project can actually help us cross three other diseases off the long list with untreatable rare diseases. The more we know, the easier it gets to develop a treatment. Which disease do we want to tackle next?
By Helena Meyer-Berg; DPhil Student; University of Oxford